I may have mentioned this before but historically, I have always been a voracious reader. I have memories of being ten and sitting down under the playground reading fictional adventure novels while kids ran around me. This happened only if the book was magically compelling, and unsurprisingly lots of YA fiction novels are at that age.
I also distinctly remember the awkward moment when at a family reunion I was hiding away under a bed reading the newest Harry Potter book when someone sat on the bed. The mattress springs crunched above me uncomfortably, so I snaked out an arm and gently tapped the family member’s ankle, sending them into an understandable jump-off-the-ground-in-total-fear-mixed-with-surprise moment. I stopped hiding under beds to read soon after that (but partially because I grew too big).
I remember years and years of trying to read during car rides while sitting in the back of my mom’s old Honda van on that way to visit some family, and feeling car sick from focusing on the words swaying about with the car’s inertia, yet still trying. I remember as an elementary school student, we had those book fairs (done by Scholastic Books I believe), which excited me to no end, and always happened in the library. I was one of those kids that liked to get some new books (and those cutesy erasers!).
As I also love things that are free (catch me in my hand-me-down clothes even as a late twenty-something mom), my love for libraries is not much of a surprise. My earliest memories of libraries are glimpses of bright light shining through musty building windows that displayed rows on rows of colorful books. I remember getting excited that I could pick out whatever I wanted, enjoying the smell of old novels, and how I loved feeling the pages of a well-worn novel. Those strong sensory experiences still continue today to evoke my love. There are also unidentified memories of accompanying adults who brought me to unfamiliar libraries on book-returning errands. And vague memories of playing those generic learning games on those chunky monitors screens.
I remember as a teen, trekking up the half mile or so from my house to the local public library, often with my friend Julia, to see what books we could find next. We had voracious appetites for fiction and fantasy, and I remember ambling through the shelves often picking books to read based on their titles or their cover art when I had no specific “to-reads” in mind. When I moved back home with my parents after college, I restarted my walking sojourns to said library, mostly to resume my enjoyment of fiction novels in between work.
I remember in high school, after tearing my ACL and not being able to run track and field senior spring, I hung out in the library with my “potluck” friends (so named because our hangouts started via a potluck meal). My grades actually improved while there so I graduated with an even higher GPA thus avoiding the stereotype of “senior slump”. And it was there that I started Pet Sematary and had my first intro to Stephen King and to more adult horror books.
While at Swarthmore I made myself a home at the Cornell science library on my free time, and started working their my sophomore year as a library assistant for work study. My now husband recalls always making sure to come chat with me when I was at the front desk as he was already crushing on me. I remember getting to work the closing shifts on nights and weekends and as a result, getting to be one of the last people in the library. I wasn’t a night person so that was often exhausting, but also a weirdly surreal experience as the building that housed the library (called the science center) was generally emptied out on weekends at that point with most of the lights off. It was quite peaceful. I remember my friend Becky and I staking our claim in a space and waiting it out in the college’s larger library (McCabe), working away until 10pm when they brought out the snacks. It was also a common library for group study as there were these study rooms on the upper floors if you wanted more privacy. I went back recently and some of the layout had changed (on the main floor at least) and it was so disorienting. Seeing a library change, even if it is for the better (which it was) is such a sucker punch to the memory.
For graduate school (MGH Institute of Health Professions in Boston) I would hide away in this renovated attic corner of the library with my friends, where we would study and sometimes practice physical therapy techniques on one another on the floor, but more often than not we would chat and enjoy life while simultaneously complaining about the breadth of material to study.
I once accompanied my husband last minute on a business trip to Ybor in Tampa, Florida. While he was doing his work thing, I decided to kill time by investigating the local library (the Robert W. Saunders Sr. Public Library). I had to walk about 2 miles to get there, and was 20 weeks pregnant, but it didn’t deter me because I always find it fascinating to see libraries in new states. I didn’t get a lot of time to explore it but I saw that it offers meals to those in need between 11:30am and 12:30pm, and it had different historical plaques and pictures about it like those below.


I also worked in the Cambridge Public Library when I was volunteering for the Eradicate Childhood Obesity Foundation and got used to navigating around one of the biggest (and oldest) library establishments in the country.
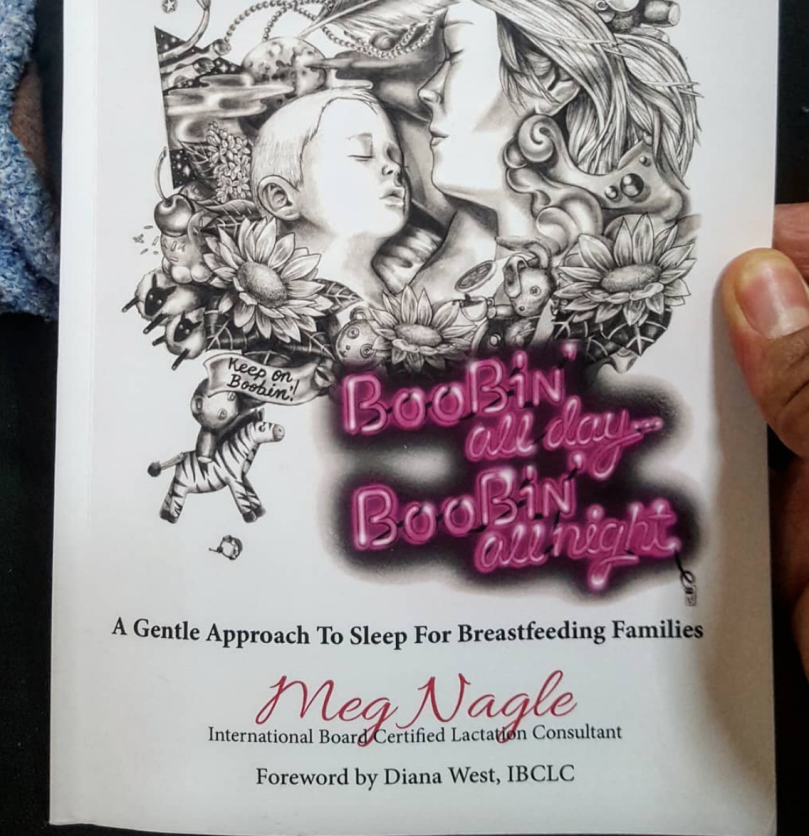
Then I visited my town library often when we briefly bought a house and lived in Swampscott, MA. After the birth of my baby, I started doing what I called drive-bys: running in to acquire books on-hold and returning the books I’ve read before taking the munchkin home. I would also, on occasion, explore the small town libraries nearby, getting jealous at some of the beautiful redone buildings and children’s sections.
When we moved to Cambridge, we lived right next to a school that had a branch of the public libraries in it, so I took Figlet to children reading events, and continued to supply my addictive habit. We also slowly were beginning to get to know other parents and nannies, with Fi starting to recognize familiar faces.
When we moved back to Maryland in November, I immediately went back to my childhood library and got a bunch of books to read, and continued in that manner until COVID-19 hit. Now, I have begrudgingly started doing e-books (still not able to do audio books because I get too distracted).
But most of all I look forward to Figlet getting older so I can see if my love of books instilled in her, and so I can spread my love of libraries and share my memories made in them while we make new ones together. She’s already started to show a taste for reading- she has a little book box that she draws from to make us read to her any time we go for naps/bedtime, or mention something she remembers us reading aloud to her. Be still, my heart!
I think part of the appeal of libraries, isn’t actually just the physical books though. For one, they usually offer ebooks and audiobooks, and CDs/DVDs, Blu-ray, journal accesses, etc (and they have branch-offs like maker spaces too). But the main reason to keep and support physical libraries is because of their environments. If they are doing it right (/if they are supported), they draw in and cater to their community. They offer computer usage and free internet to all and they hold events to enrich, educate, and encourage new skills and passions. They provide a safe place to stay if you can’t go home right away, or a place to go and study/get work done if you just need a change of pace. In an age where people don’t invest as much time in their towns in a larger centralized social sort of way, where community centers may not always exist, one can usually rely on their public library to be a get-together place. And if they don’t have something offered you want, they usually are receptive to feedback. These are traits that cannot be replaced by Amazon stores or online shopping.
For those interested, the book, Bibliotech: Why Libraries Matter More Than Ever in the Age of Google by John Palfrey goes into more detail about multiple reasons that libraries are important.
I also have started thinking more about the models of book-sharing and used books, and started to appreciate companies like Wonder Books, that take books no one else wants and try to keep them from being shredded (including from libraries!) I also love love love the free libraries outside on people’s yards and think they are cute way to share books in a hyper-local environment. Maybe library’s could start setting up Free Libraries at parks or areas that aren’t as well stocked with books to find new homes for the books the library might be planning to throw out?